Hemorrhoid Treatment Specialist NYC | New York City Hemorrhoid Doctor
Our board-certified gastroenterologists are experts in non-surgical hemorrhoid treatments offering safe and effective same-day removal in Midtown & Upper East Side NYC.
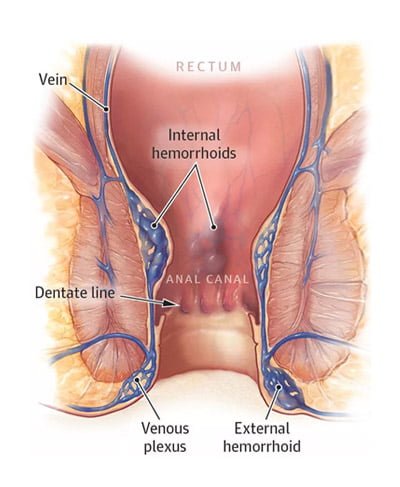
Diagram-of-hemorrhoids – Orange County Hemorrhoid Clinic
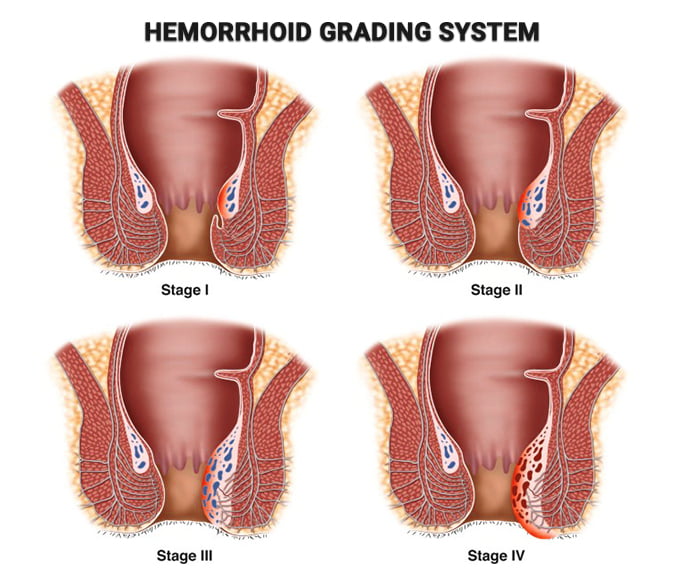
Hemorrhoid Grading System – Manhattan Gastroenterology
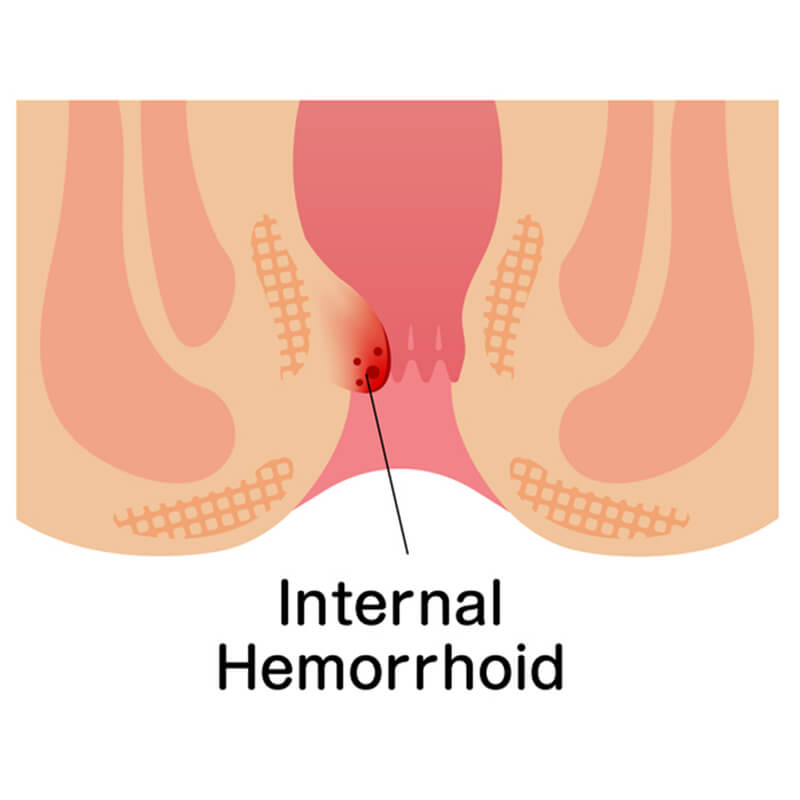
Hemorrhoids are a regular part of your everyday anatomy. They are clusters of venous structures in the rectal area. They acts like vascular cushions, protect the anal sphincter and aid closure of the anal canal during increased abdominal pressure.

External hemorrhoids: Treatment, pictures, symptoms, and causes Medical News Today
An external hemorrhoid is a hemorrhoid that occurs outside of the body in the veins around the anus. Learn more about the symptoms, causes, and treatments here.

HEMORRHOIDS | Matthew Johnson MD, FACS
HEMORRHOIDS Hemorrhoids are not life-threatening, but they can make life miserable for some people. Internal and External Hemorrhoids Internal hemorrhoids are far enough inside the rectum th…
Hemorrhoids FAQs
Options for hemorrhoid treatment during colonoscopy

I’ve been suffering from grade 1 hemorrhoids for the past 8 years. What should I do? – Quora
Answer (1 of 11): ** Hemorrhoids Pictures, Causes, Symptoms, and Cure ** Quora required LINK: Hemorrhoids Pictures, Causes, Symptoms, and Cure . Grade 1: The internal hemorrhoid bulges into the canal but does not prolapse or fall completely into it. … * Grade 2: The hemorrhoid protrude…

THE HEMORRHOIDS GRADING SYSTEM GUIDE. HEMORRHOID GRADE SCALE 1, 2, 3, – REVIVOL-XR
Hemorrhoid Grade 1, 2, 3, 4 Hemorrhoid Grading System Stages of Hemorrhoids I II III IIII Grades of Hemorrhoids Grade 4 Hemorrhoids Grade 3 Hemorrhoids Grade 2 Hemorrhoids Grade 1 Hemorrhoids Hemorrhoids Size Chart Internal External Classification Prolapsed Skin Tag Fissure Treatment Treating hemorrhoidal disease

Hemorrhoid – Wikipedia

Hemorrhoids
痔疮 Buasir/ Wasir -Refer Manipal pg 792 It is 3 cm long, staits as the continuation of rectum, passes through pelvic diaphragm and ends at the anal verge (skin…
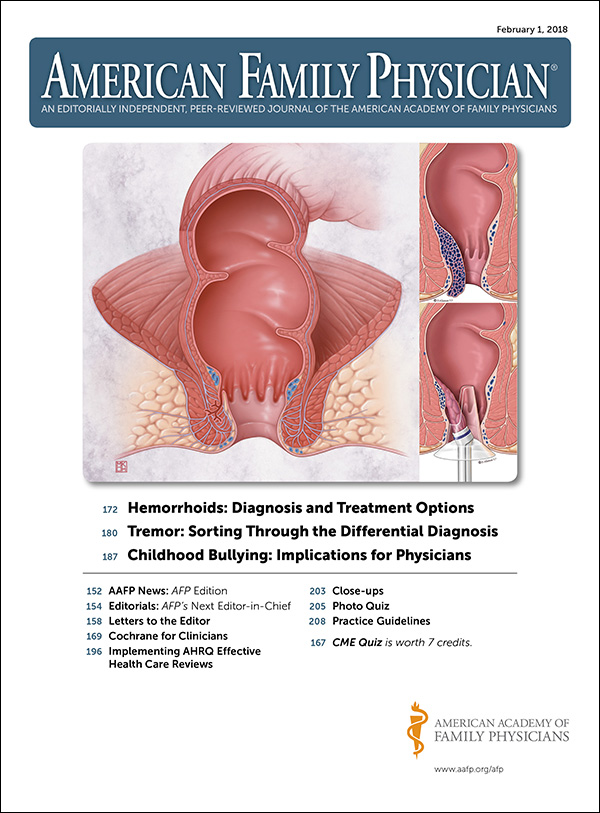
Hemorrhoids: Diagnosis and Treatment Options | AAFP
Many Americans between 45 and 65 years of age experience hemorrhoids. Hemorrhoidal size, thrombosis, and location (i.e., proximal or distal to the dentate line) determine the extent of pain or discomfort. The history and physical examination must assess for risk factors and clinical signs indicating more concerning disease processes. Internal hemorrhoids are traditionally graded from I to IV based on the extent of prolapse. Other factors such as degree of discomfort, bleeding, comorbidities, and patient preference should help determine the order in which treatments are pursued. Medical management (e.g., stool softeners, topical over-the-counter preparations, topical nitroglycerine), dietary modifications (e.g., increased fiber and water intake), and behavioral therapies (sitz baths) are the mainstays of initial therapy. If these are unsuccessful, office-based treatment of grades I to III internal hemorrhoids with rubber band ligation is the preferred next step because it has a lower failure rate than infrared photocoagulation. Open or closed (conventional) excisional hemorrhoidectomy leads to greater surgical success rates but also incurs more pain and a prolonged recovery than office-based procedures; therefore, hemorrhoidectomy should be reserved for recurrent or higher-grade disease. Closed hemorrhoidectomy with diathermic or ultrasonic cutting devices may decrease bleeding and pain. Stapled hemorrhoidopexy elevates grade III or IV hemorrhoids to their normal anatomic position by removing a band of proximal mucosal tissue; however, this procedure has several potential postoperative complications. Hemorrhoidal artery ligation may be useful in grade II or III hemorrhoids because patients may experience less pain and recover more quickly. Excision of thrombosed external hemorrhoids can greatly reduce pain if performed within the first two to three days of symptoms.

What Do Hemorrhoids Look Like: Types and More Healthline
There are four types of hemorrhoids: internal, external, prolapsed, and thrombosed. Find out what they look like and more.

Hemorrhoids: Causes, treatments, and prevention Medical News Today
Hemorrhoids, or piles, are common irritations around the rectum and can be extremely painful. Learn about what causes hemorrhoids, how to avoid them, home remedies, and when to see a doctor.
Hemorrhoids: Diagnosis and Treatment Options | AAFP
Many Americans between 45 and 65 years of age experience hemorrhoids. Hemorrhoidal size, thrombosis, and location (i.e., proximal or distal to the dentate line) determine the extent of pain or discomfort. The history and physical examination must assess for risk factors and clinical signs indicating more concerning disease processes. Internal hemorrhoids are traditionally graded from I to IV based on the extent of prolapse. Other factors such as degree of discomfort, bleeding, comorbidities, and patient preference should help determine the order in which treatments are pursued. Medical management (e.g., stool softeners, topical over-the-counter preparations, topical nitroglycerine), dietary modifications (e.g., increased fiber and water intake), and behavioral therapies (sitz baths) are the mainstays of initial therapy. If these are unsuccessful, office-based treatment of grades I to III internal hemorrhoids with rubber band ligation is the preferred next step because it has a lower failure rate than infrared photocoagulation. Open or closed (conventional) excisional hemorrhoidectomy leads to greater surgical success rates but also incurs more pain and a prolonged recovery than office-based procedures; therefore, hemorrhoidectomy should be reserved for recurrent or higher-grade disease. Closed hemorrhoidectomy with diathermic or ultrasonic cutting devices may decrease bleeding and pain. Stapled hemorrhoidopexy elevates grade III or IV hemorrhoids to their normal anatomic position by removing a band of proximal mucosal tissue; however, this procedure has several potential postoperative complications. Hemorrhoidal artery ligation may be useful in grade II or III hemorrhoids because patients may experience less pain and recover more quickly. Excision of thrombosed external hemorrhoids can greatly reduce pain if performed within the first two to three days of symptoms.
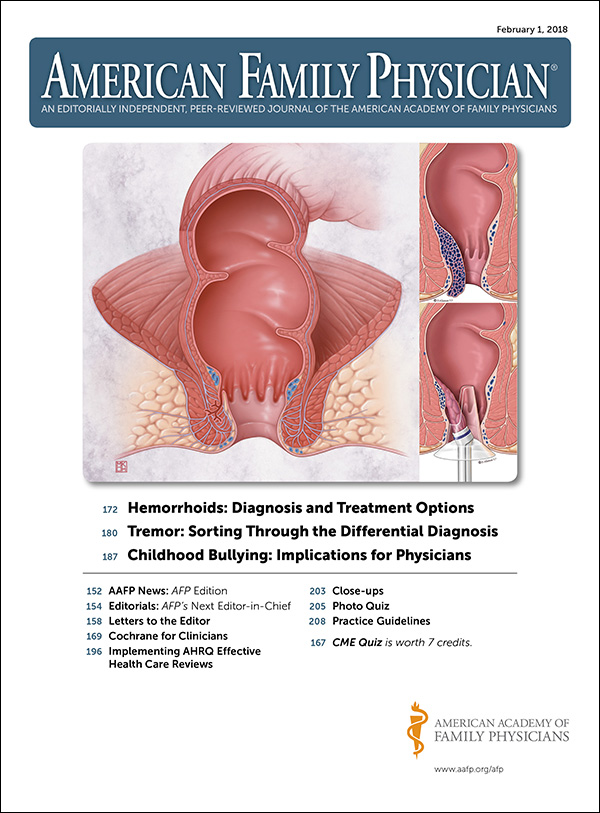
Hemorrhoids: Diagnosis and Treatment Options | AAFP
Many Americans between 45 and 65 years of age experience hemorrhoids. Hemorrhoidal size, thrombosis, and location (i.e., proximal or distal to the dentate line) determine the extent of pain or discomfort. The history and physical examination must assess for risk factors and clinical signs indicating more concerning disease processes. Internal hemorrhoids are traditionally graded from I to IV based on the extent of prolapse. Other factors such as degree of discomfort, bleeding, comorbidities, and patient preference should help determine the order in which treatments are pursued. Medical management (e.g., stool softeners, topical over-the-counter preparations, topical nitroglycerine), dietary modifications (e.g., increased fiber and water intake), and behavioral therapies (sitz baths) are the mainstays of initial therapy. If these are unsuccessful, office-based treatment of grades I to III internal hemorrhoids with rubber band ligation is the preferred next step because it has a lower failure rate than infrared photocoagulation. Open or closed (conventional) excisional hemorrhoidectomy leads to greater surgical success rates but also incurs more pain and a prolonged recovery than office-based procedures; therefore, hemorrhoidectomy should be reserved for recurrent or higher-grade disease. Closed hemorrhoidectomy with diathermic or ultrasonic cutting devices may decrease bleeding and pain. Stapled hemorrhoidopexy elevates grade III or IV hemorrhoids to their normal anatomic position by removing a band of proximal mucosal tissue; however, this procedure has several potential postoperative complications. Hemorrhoidal artery ligation may be useful in grade II or III hemorrhoids because patients may experience less pain and recover more quickly. Excision of thrombosed external hemorrhoids can greatly reduce pain if performed within the first two to three days of symptoms.

Treating hemorrhoidal disease: Conservative vs. surgical approaches | Digestive | UT Southwestern Medical Center Appointment Appointment Appointment Appointment Call Appointment Share via Facebook Share via Twitter Share via LinkedIn Share via Email Print this page Facebook Twitter YouTube
Hemorrhoidal disease affects about 10 million people per year in the U.S., but many people arent aware of the many effective treatment options that are available.

Figure 3 from Hemorrhoids: Diagnosis and Treatment Options. | Semantic Scholar Semantic Scholar Semantic Scholar
FIGURE 3 – Hemorrhoids: Diagnosis and Treatment Options.
Best Ayurvedic medicine for piles | Piles Capsule | Piles treatment
Piles Medicine,Best Medicine for Piles,Piles Treatment Medicine,Piles Cure medicine,Piles Cure Treatment,Piles Treatment Capsules,Ayurvedic Fissure Medicine,Ayurvedic Medicine for Fistula

Size Chart
Shop our natural products for warts treatment, skin tag removal, skin mole remover, hemorrhoids treatment, scar removal and varicose veins treatments today!
Hemorrhoids Surgical Devices Market – Global Industry Trends and Forecast to 2028 | Data Bridge Market Research Search
Global Hemorrhoids Surgical Devices Market, By Device (Band Ligators (Endoscopic Ligators, Non-endoscopic Ligators), Sclerotherapy Injectors, Infrared Coagulators, Bipolar Probes, Cryotherapy Devices, Hemorrhoid Laser Probes), Hemorrhoid Type (Internal Hemorrhoids, External Hemorrhoids), End Users (Hospitals, Homecare, Specialty Clinics, Others), Country (U.S., Canada, Mexico, Germany, Italy, U.K., France, Spain, Netherland, Belgium, Switzerland, Turkey, Russia, Rest of Europe, Japan, China, India, South Korea, Australia, Singapore, Malaysia, Thailand, Indonesia, Philippines, Rest of Asia-Pacific, Brazil, Argentina, Rest of South America, South Africa, Saudi Arabia, UAE, Egypt, Israel, Rest of Middle East & Africa) Industry Trends and Forecast to 2028

Immuno | Free Full-Text | Anti-Inflammatory, Antimicrobial, and Vasoconstriction Activities of an Anti-Hemorrhoidal Mixture of Alchemilla vulgaris, Conyza bonariensis, and Nigella sativa: In Vitro and Clinical Evaluations
Nigella sativa, Conyza bonariensis, and Alchemilla vulgaris are highly recommended in Greco-Arab traditional medicine as anti-hemorrhoid medicinal plants. The efficacy and safety of a topical cream (HPC) consisting of water–ethanol extracts of these three plants were evaluated here in vitro and in a randomized, double-blind, placebo-controlled study (RDBPC). HPC showed no significant cytotoxic effects in fibroblast cell line 3T3 (LDH-release and MTT assay); it inhibited the nitric oxide production by cultured monocyte cell line THP-1 in a dose-dependent manner (reaching the control levels of untreated cells at a concentration of 100 μg/mL). HPC showed a dose-dependent antibacterial activity against Escherichia coli (60% inhibition compared to Ampicillin at 5 mg/disc) and a significant vasoconstriction effect on intestinal vein rings (40% increase compared to phenylephrine). In a RDBPC with 77 hemorrhoidal disease (patients ages 19–61 years with a median grade of hemorrhoids of 2.0), we determined the anti-hemorrhoid efficacy and safety of HPC. The patients were randomly assigned to the HPC group (54 patients) or the placebo group (23 patients). They were asked to apply 2–3 mL of HPC or placebo twice daily for 6 days. The degree of hemorrhoidal disease severity, hemorrhage severity, pain, and itching served as an evaluation of the HPC efficacy. Compared to the placebo group, the obtained results showed that 6 days of treatment with HPC reduced the indexes of hemorrhage severity, severity of pain, and severity of itching to 0–1, 1, and 1 after 6 days, respectively. In conclusion, patients treated with HPC had a significant clinical improvement in all disease severity parameters compared to placebo. In vitro evaluations proved HPC to have significant antimicrobial, anti-inflammatory, and vasoconstriction effects. Therefore, HPC represents an interesting alternative treatment for hemorrhoidal disease.
Europe PMC Europe PMC
Europe PMC is an archive of life sciences journal literature.
Overcoming fiber dependence
Dietary fiber is literally a delayed-fuse mine inside your gut. This guide explains how to overcome dependence on fiber without resorting to laxatives.
Hemorrhoid Treatment Calgary | N.A. Hemorrhoid Centre
Our hemorrhoid treatment gets to the root of the problem so you can start living your pain-free life today! Contact us today!

Hemorrhoids: The Definitive Guide to Medical and Surgical Treatment – Consult QD Left Arrow Right Arrow email email
Heres a comprehensive review of how to diagnose and grade hemorrhoids, as well as how to select the appropriate medical or surgical treatment based on current clinical evidence.
How do you Reduce the Size of Your Hemorrhoids? | GI Associates
External Hemorrhoids, Why Are They Popping Out? External hemorrhoids, also called piles, are swollen veins in the anal canal. They can form when you…
Hemorrhoids: Diagnosis and Treatment Options | AAFP
Many Americans between 45 and 65 years of age experience hemorrhoids. Hemorrhoidal size, thrombosis, and location (i.e., proximal or distal to the dentate line) determine the extent of pain or discomfort. The history and physical examination must assess for risk factors and clinical signs indicating more concerning disease processes. Internal hemorrhoids are traditionally graded from I to IV based on the extent of prolapse. Other factors such as degree of discomfort, bleeding, comorbidities, and patient preference should help determine the order in which treatments are pursued. Medical management (e.g., stool softeners, topical over-the-counter preparations, topical nitroglycerine), dietary modifications (e.g., increased fiber and water intake), and behavioral therapies (sitz baths) are the mainstays of initial therapy. If these are unsuccessful, office-based treatment of grades I to III internal hemorrhoids with rubber band ligation is the preferred next step because it has a lower failure rate than infrared photocoagulation. Open or closed (conventional) excisional hemorrhoidectomy leads to greater surgical success rates but also incurs more pain and a prolonged recovery than office-based procedures; therefore, hemorrhoidectomy should be reserved for recurrent or higher-grade disease. Closed hemorrhoidectomy with diathermic or ultrasonic cutting devices may decrease bleeding and pain. Stapled hemorrhoidopexy elevates grade III or IV hemorrhoids to their normal anatomic position by removing a band of proximal mucosal tissue; however, this procedure has several potential postoperative complications. Hemorrhoidal artery ligation may be useful in grade II or III hemorrhoids because patients may experience less pain and recover more quickly. Excision of thrombosed external hemorrhoids can greatly reduce pain if performed within the first two to three days of symptoms.

Diet Chart For Piles Patient, Piles Diet Chart chart | Lybrate.
Diet chart for Piles patient and a healthy life. Find balanced diet chart for Piles Patient, Learn more about Piles Diet Chart chart from the experts at Lybrate.

Are hemorrhoids genetic? | Decode your DNA and learn your risks!
Are hemorrhoids genetic? Hemorrhoids are enlarged blood vessels in the anus and lower rectum that can become painful if left untreated.

Clinics and Practice | Free Full-Text | Increased Risk of Bleeding with Topical Metronidazole in a Postoperative Wound after Anal Fistula and Hemorrhoid Surgery: A Propensity Score-Matched Case–Control Study
Background: Topical metronidazole (TM) is commonly used in many infective conditions and postoperative wounds including after anorectal surgery. TM was prescribed in patients operated for benign anorectal conditions (anal fistula and hemorrhoids) to hasten wound healing. After the initiation of this protocol, the incidence of postoperative wound bleeding seemed to increase. There are no data in the literature suggesting that topical metronidazole increases the risk of bleeding. Objective: Analysis of the association of TM with an increased risk of bleeding in postoperative anorectal wounds. Design: This was an observational and a retrospective study. Propensity score matching was performed. Setting: This study was conducted at a specialized center for anorectal disorders in postoperative patients suffering from anal fistula and hemorrhoids. Materials: The incidence of postoperative bleeding in the patients in whom TM was used (study group) was retrospectively compared with the patients operated one year before this period in whom TM was not used (control group). Sample size: There were 35 patients in the study group and 181 patients in the control group. Main outcome measures: The incidence of bleeding and the number of bleeding episodes were evaluated. Results: The incidence of bleeding was significantly higher in the study group as compared to the control group (8/35 (22.8%) vs. 8/181 (4.4%), respectively, p = 0.0011). In most cases, bleeding was controlled with conservative measures. The number of bleeding episodes was also significantly higher in the study group (14 vs. 11, respectively, p = 0.0001). The number of patients requiring operative intervention was also higher in the study group (2/35—5.7%) as compared to the control group (1/181—0.56%), but this was not statistically significant (p = 0.069). Conclusions: The study highlighted that application of topical metronidazole in postoperative anorectal wounds increased the risk of bleeding. Most of the bleeding episodes were controlled with conservative measures but they caused considerable patient anxiety and apprehension.

Transanal hemorrhoidal dearterialization: Lessons learned from a personal series of 200 consecutive cases and a proposal for a tailor-made procedure – ScienceDirect ScienceDirect
Transanal hemorrhoidal dearterialization (THD) is an effective treatment for hemorrhoidal disease (HD). However, the surgical technique is not standar…

Frontiers | Self-Mechanical Anal Dilatation: A Simple Trick to Minimize Postoperative Pain and Stenosis Following Hemorrhoidectomy With Radiofrequency
Aim: Hemorrhoidectomy is still the most effective surgical treatment for hemorrhoidal disease, but it is, however, associated with complications such as pain and stenosis. We proposed to break the vicious circle of pain–sphincteric spasm–stenosis–pain with the postoperative use of self-mechanical anal dilation.Methods: We retrospectively analyzed patients with hemorrhoidal disease presenting with a minimum of piles of three quadrants, treated with radiofrequency hemorrhoidectomy between January 2018 and December 2019. All the patients that at 3 weeks presented sphincteric spasms with painful defecation, were considered. Thirty-nine patients performed the cycle of self-mechanical anal dilation (Group A). This group was 1:1 matched with homogeneous patients from our historical cohort of patients (Group B). The primary endpoint was the pain evaluation, secondary endpoints: WCS, overall satisfaction of the patient, anal sphincter spasm, scarring, and the incidence of postoperative stenosis.Results: In Group A mean VAS was 3.25 after 14 days of application and 1.15 at the end of the application. In Group B mean VAS was persistently higher, with a mean VAS of 5 (p = 0.000002) and 3.38 (p = 0.0000000000009). In Group A we observed an improvement of symptoms at the end, with a good overall satisfaction (Group A 7.4 vs. Group B 5.9; p = 0.0000007) and a better mean WCS (Group A WCS 2.8 vs. Group B WCS 4.18; p = 0.0001). Stenosis was observed in 3/39 patients of Group B (7.7%).C…
